You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Historically, many general dentists have felt that providing dental implant treatments is beyond the capacity of their private practices. However, with proper education and training, understanding key factors essential for implant treatment success, and appropriate case selection, dental implants can be a component of virtually any general dentist’s treatment offerings. Dentists may choose to either focus exclusively on restoring implants—as many dentists do—or perform both implant placement and subsequent restoration.
To facilitate the process, dentists can take steps to properly plan implant placement and angulation based on an understanding of available bone quantity, quality, and space, and then select the most appropriate implant and related restorative components. This can help to ensure precise implant location, as well as an intimate fit and connection between the implant, abutment, and restoration.
An example illustrating the manner in which these factors are considered in case selection, implant placement, and implant restoration is the case of a female patient who presented with a missing central incisor, tooth No. 8 (Figure 1 and Figure 2). While this example presents an ideal situation for a single implant-supported restoration, analysis is required to determine the appropriate implant width and length, presence of adequate bone, quality and quantity, soft-tissue health, abutment type (ie, custom or stock), and restoration type (ie, cement- or screw-retained).
Determining Implant Width
Because implants are available in a variety of widths and lengths, an analysis of average tooth widths is helpful in the context of implant selection. For example, a fully anatomical central incisor is approximately 8.6 mm wide (Figure 3). However, determining the implant size requires understanding a 3-dimensional, cross-sectional perspective encompassing the gingival crest, cemento-enamel junction (CEJ), and available and required space for both the implant and the planned restoration.1,2
The depth of the implant ultimately determines the dimensions of the restoration, and such factors as bone and soft-tissue quality, as well as the cervical contours of the restoration, will affect integration of the entire treatment.1,2 Ideally, the top of an implant for replacing a central incisor should be positioned 3 mm to 4 mm below the gingival crest, which is approximately 2 mm below the CEJ; this represents the beginning of the restorative interface. This suggests that a root—or implant—diameter of approximately 5.5 mm wide would be appropriate.1,2
However, when selecting between a 4.3-mm implant and a 5-mm implant, considerations regarding which would position better are significant. A 4.3-mm implant would seat precisely in the middle of the 8.6-mm width, leaving 4.3 mm of space/surface area for building the restoration between adjacent teeth contacts (ie, 2.15 mm on either side). This would provide sufficient support for the bone/ implant interface to resist occlusal forces and allow surgical access.
This type of preoperative implant selection and placement planning, which can be conducted for all teeth anteriorly to posteriorly in a similar manner on a site-by-site basis, ensures a predictable, functional, esthetic, and biologically stable outcome.3 Space requirements for restoration, preserving and maintaining available bone and soft tissue, and ensuring adequate support against occlusal forces remain among the considerations when determining implant length and width to avoid compromises.4
Implant Placement
Radiographic examination of the site for implant placement is essential to determine the presence of adequate space for the implant and subsequent restoration (eg, central incisor) and to assess soft-tissue architecture.1,2 Computed tomography (CT) images and panoramic radiographs (eg, panorex) have been used in implant dentistry to help identify structures critical for implant placement and establish the safe, short distance for implant placement (ie, vertical control of implant placement) using a pilot drill (Figure 4).5
A flap procedure reveals the bone, which should be wide enough to provide 1.5 mm of bone on either side of the implant (Figure 5).6 The amount and level of bone surrounding implants is important for osseointegration, esthetics, and long-term survival.6 The location for implant placement can then be established using a round bur to place a mark in the center of the crest of bone from mesial-distally and facial-palatally (Figure 6).
Implant Length Selection
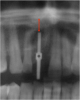
Pilot drills, which are typically 2 mm wide, are used to drill into the trajectory of the bone to a short, safe distance to establish position and angulation (Figure 7). Care must be taken to observe the premaxilla angulation, which averages 20 degrees. Then, a direction-indicating pin is placed (Figure 8) and a radiographic image is taken (Figure 9).7 This image (eg, panorex) is enlarged to enable further analysis and measurements, particularly to establish the exact height of bone.
The approximate 20% horizontal and vertical distortion is calculated.4 This can be accomplished by measuring from the top of the guide pin to the opposing vital structure (eg, floor of the nose, 5 mm). Because of the 20% distortion, the actual measurement is 4 mm. Thus, there is a total of 14 mm of vertical bone height (ie, 10 mm for the length of the pin, plus 4 mm to the floor of the nose), and a 13-mm-length implant would be selected.
A similar procedure could be employed when determining bone height and implant length for other implant site locations in the posterior. However, anatomical landmarks (eg, nerve locations) require additional considerations. Usually 4 mm of height is left between the inferior alveolar nerve and the implant.4
Osteotomy and Implant Insertion
Different implants require the use of different drill kits for widening the osteotomy when going to depth. In the present case, the osteotomy is initially widened to 3.5 mm and taken to a depth of 11 mm (Figure 10), after which a different drill will be used to widen it to 4.3 mm and increase the depth to 13 mm to accommodate the selected implant (Figure 11).7 The implant is then inserted and properly torqued to 35 Ncm, after which a healing abutment is placed (Figure 12).
Restoring Implants
Following osseointegration, the first step in implant restoration is making an impression of an impression coping, the adjacent and opposing teeth, and the surrounding soft tissue in order to fabricate an esthetic and functional restoration. The healing abutment is removed (Figure 13), an impression coping is screwed into place with a drop-and-lock anti-rotation (Figure 14), and a radiograph is taken to ensure the implant is fully seated. Then, an impression is made by expressing a medium-body impression material around the impression coping (Figure 15) and placing a stock tray filled with putty in the mouth (Figure 16). To obtain an accurate impression, the tray is fully seated with slight pressure, and the tray is removed when set and the impression inspected for accuracy.
Following impression-making, the healing abutment can be reseated, and/or a provisional abutment/restoration placed. During provisionalization, a laboratory fabricates the final abutment and restoration based on the impression received, shade selection provided by the dentist, and type of final restoration desired.
Abutment Selection
Implant abutments function like conventional crown-and-bridge preparations and, in fact, are crown preparations for screw-retained implants. In theory, implant abutments should demonstrate the same design principles as natural tooth preparations (ie, proper emergence through the soft tissues so that cementation margins rest at the correct height; proper margination; ideal occlusal reduction taper).
When selecting an abutment for a given case, factors for consideration include the level of restorative support required, periodontal stability, esthetics, and ability to facilitate oral hygiene.3 Additionally, other implant abutment criteria include implant position and angulation, soft-tissue height and contours, and interocclusal space.8 The types of abutments available today include custom abutments and prefabricated stock abutments (Figure 17), as well as those for either screw-retained or cement-retained restorations.
Custom Abutments—Custom abutments have been associated with ideal preparation designs, marginal integrity, proper axial walls, and proper occlusal reduction. Because custom abutments are designed for the individual case, implant site, and restoration, the margin heights can be tailored to the restoration and surrounding tissue, as well as placed in the ideal location (ie, supragingival, subgingival, or equigingival). When used with cement-retained restorations, custom abutments have demonstrated sufficient stability to support all-ceramic restorations in the anterior region, with favorable soft- and hard-tissue reactions.9,10
Stock Abutments—Prefabricated stock abutments do not demonstrate customized margin heights, tapers, or incisal/occlusal reductions. In fact, the occlusal/incisal reduction is typically only 1:1. Because prefabricated abutments do not generally follow the patient’s gingival contours, there is a lack of support for the emergence profile.
Restoration Design
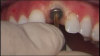
Single implants can be restored with either cement-retained or screw-retained restorations. With cement-retained restorations, the abutment is first screwed and torqued into place, after which the crown restoration is cemented onto it (Figure 18). If a screw-retained option is used, the restoration is retained via a screw-access hole that has typically been placed on the occlusal aspect. After restoration placement, this access channel is sealed with composite. However, anterior screw-retained restorations historically have been challenging for dentists due to the incisal/facial location of the access hole. With the recent development of a 25-degree screw channel from the long axis of the implant, the access hole can be placed on the lingual or cingulum for anterior restorations (Figure 19 and Figure 20). Additionally, such angulation could also facilitate screw retention of posterior restorations in which mouth opening and/or access is limited.
When deciding between cement-retained or screw-retained implant restorations, the clinician should bear in mind that controversy and conflicting reports surround each type, and advantages and disadvantages have been cited for each.11,12 The type of abutment used for cement- and screw-retained implant restorations influences many aspects of clinical success, as well as the passivity of the restoration framework, occlusion, and retention overall.12,13 Interestingly, systematic reviews have shown little significant difference between cement- and screw-retained restorations for major and minor outcomes (eg, implant loss, crown loss, screw loosening, decementation, porcelain fracture), suggesting that neither is inferior.14,15
Laboratory Fabrication
Once the laboratory receives the impression and instructions regarding abutment selection, restoration design/type, and desired shades, the impressions are scanned and/or otherwise used for fabricating the implant-supported restoration and abutment. This includes creating models to verify fit and contacts (Figure 21). If a screw-retained restoration is selected, software is used to calculate and determine the proper angulation of the screw channel, and the restoration and abutment are fabricated to offset that to the cingulum. In the case of the female patient who presented with the missing tooth No. 8, the restoration was fabricated and placed to be a mirror image of the adjacent natural tooth, with proper soft-tissue architecture (Figure 22).
Conclusion
The keys to successful implant dentistry for general dentists are training, case selection, understanding procedure, and realizing when it is appropriate to refer out difficult or complex cases. Many patients with one or more missing teeth may be candidates for implant treatments, and general dentists can provide these services. In particular, general dentists can place implants and restore them, or simply provide the restoration(s). Either way, understanding the steps required to properly plan implant placement and angulation, determine available bone quantity, quality, and space, and considerations for selecting the most appropriate implant and related restorative components (eg, stock or custom abutment, cement- or screw-retained restoration) can help to ensure predictable implant restoration outcomes.
ABOUT THE AUTHOR
Ken Hebel, DDS
Private Practice, London, Ontario, Canada
REFERENCES
1. Hebel KS, Gajjar RC. Achieving superior aesthetic results: parameters for implant and abutment selection. Int J Dent Symp. 1997;4(1):42-47.
2. Hebel KS, Gajjar RC. Anatomic basis for implant selection and positioning. In: Babbush CA, Hahn JA, Krauser JT, Rosenlicht JL. Dental Implants: The Art and Science. Philadelphia, Pa: Elsevier; 2000:85-103.
3. Solow RA. Clinical considerations for selecting implant abutments for fixed prosthodontics. Gen Dent. 2015;63(1):30-36.
4. Kalra M, Aparna IN, Dhanasekar B. Evolution of surgical guidance in implant dentistry. Dent Update. 2013;40(7):577-578,581-582.
5. de Brito AC, Nejaim Y, de Freitas DQ, de Oliveira Santos C. Panoramic radiographs underestimate extensions of the anterior loop and mandibular incisive canal. Imaging Sci Dent. 2016;46(3):159-165.
6. Prasad DK, Shetty M, Bansal N, Hegde C. Crestal bone preservation: a review of different approaches for successful implant therapy. Indian J Dent Res. 2011;22(2):317-323.
7. Weinberg LA, Kruger B. Three-dimensional guidance system for implant insertion: Part 1. Implant Dent. 1998;7(2):81-93.
8. Giglio GD. Abutment selection in implant-supported fixed prosthodontics. Int J Periodontics Restorative Dent. 1999;19(3):233-241.
9. Vanlıoglu BA, Özkan Y, Evren B, Özkan YK. Experimental custom-made zirconia abutments for narrow implants in esthetically demanding regions: a 5-year follow-up. Int J Oral Maxillofac Implants. 2012;27(5):1239-1242.
10. Hjerppe J, Lassila LV, Rakkolainen T, et al. Load-bearing capacity of custom-made versus prefabricated commercially available zirconia abutments. Int J Oral Maxillofac Implants. 2011;26(1):132-138.
11. Wittneben JG, Millen C, Brägger U. Clinical performance of screw- versus cement-retained fixed implant-supported reconstructions—a systematic review. Int J Oral Maxillofac Implants. 2014;29 suppl:84-98.
12. Michalakis KX, Hirayama H, Garefis PD. Cement-retained versus screw-retained implant restorations: a critical review. Int J Oral Maxillofac Implants. 2003;18(5):719-728.
13. Lee A, Okayasu K, Wang HL. Screw-versus cement-retained implant restorations: current concepts. Implant Dent. 2010;19(1):8-15.
14. Sherif S, Susarla HK, Kapos T, et al. A systematic review of screw- versus cement-retained implant-supported fixed restorations. J Prosthodont. 2014;23(1):1-9.
15. Lemos CA, de Souza Batista VE, Almeida DA, et al. Evaluation of cement-retained versus screw-retained implant-supported restorations for marginal bone loss: A systematic review and meta-analysis. J Prosthet Dent. 2016;115(4):419-427.