You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Imaging guidance in detecting periapical pathology, searching for natural dentition root fractures, evaluating periodontal defects, and identifying jaw bone volume are predominantly diagnosed by examination and standard 2-dimensional (2D) radiographs. However, when diagnosing and treatment planning long-term restorations, more detailed information is required with 3-dimensional (3D) images, which can be provided for preoperative planning by conventional computerized tomography (CT). Going further, cone-beam computed tomography (CBCT), which provides a new class of 3D images, gives promising results in determining facial structures and the presence of defects. CBCT has been used as a new method for maxillofacial imaging; it produces images with a high diagnostic quality and isotropic submillimeter spatial resolution, and it has a lower radiation dose and shorter scanning time than conventional CT.1,2 To date, CBCT has been widely used for the assessment of temporomandibular joints, trauma of the facial skeleton, endodontic periapical pathology, and dental implant planning.3
It is important for dentists to have an understanding of the utilization of CBCT compared with standard 2D radiography. Standard 2D radiography provides an approximation of possibilities of pathology, periodontal defects, and implant position. 3D images allow precise mapping of maxillary and mandibular structures and can be reproduced in presenting images for even small fractures of natural dentition and alveolar structures.4 CBCT is not only superior by providing 3D image views, it exhibits the capability of lower radiation than conventional CT-CBCT suits the principle of "as low as reasonably achievable" (ALARA). This guiding principle of radiation safety means that even if a dose is small, if receiving that dose has no direct benefit, it should be avoided.5
For any patient who presents to a dental practice with limited opening and an inability to have traditional intraoral radiographs taken, CBCT expedites the evaluation of the condition. CBCT radiography also aids in detecting the nature of less-obvious infections and fractures with associated symptoms (eg, pain). Without CBCT views, clinical signs and symptoms that present possibilities of fractures and infection can result in unpredictable conditions if they were unable to be confirmed with 2D radiographs. This situation often presents in dental practices. For example: a patient reports to the practice with pain and swelling of the lower-left first-molar region. A periapical or panoramic radiograph is ordered (2D radiographs). On review, the images do not reveal much if any changes in bone, radiolucency, or fracture. 2D images are delivered in a parallel beam directed from the buccal to the lingual, then imaged onto the sensor and reported back to one's computer monitor. The software calculates the information with averages of the pixels received after exposure to radiation. If the patient has a particularly thick buccal-bone profile, the image would suggest no periapical pathology or root fracture. Taking into consideration that CBCT is a volumetric 360-degree lower-energy radiograph, the data that are sent to the software for calculation produce a more accurate image based on algorithms within the software.
Advantages of CBCT, which include its lower dose of radiation than conventional CT, its improved accuracy in identifying fractures, and the relatively lower radiation exposure compared with plain radiographs, support the use of this method for maxillofacial imaging.6 Recently, CBCT has been widely used for image-guided surgery because the images show sufficient pertinent anatomy and pathology. The author advocates using CBCT in addition to plain radiographs in assessing a complex region such as the facial. In most situations, CBCT is only an adjunct investigation that helps supplement clinical and standard radiographic investigations.
Dental implants along with sophisticated dental laboratory support have revolutionized restorative dentistry. Dental-implant popularity and a large acceptance have led to a point where implants have become an alternative and routine option in oral-rehabilitation treatment planning. CBCT imaging plays a vital role in guiding a clinician in diagnosing, treatment planning, and case presentation.
Utmost consideration should be given to the fact that patients come to see their dentists to buy back their smile. Patients want teeth; they do not want sinus elevations and bone grafting with endosseous dental implants associated with fixed or removable prostheses. To perform successful CBCT imaging, one must recognize that the imaging and the smile/teeth that patients request are driven by prosthetics. The ultimate objective of implant placement is a fundamental esthetic and maintainable long-term restoration.7
When to Save or Remove
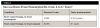
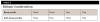
Assuming a natural tooth is restorable, considerations should include the conditions surrounding the tooth and what the patient is willing to accept as treatment. Literature has cited root canal parameters for initial therapy, re-treatment, initial apical surgery, and subsequent apical surgeries.8 Table 1 shows a longitudinal study regarding success rates 2 to 4 years after treatment; Table 2 shows a greater decline in success rates 4 to 6 years postoperatively. (No articles evaluated success rates for nonsurgical therapy after 6 years. Articles discussed survival rates. If the tooth is still in the mouth and without pain, it is questionable for restoration placement.)
The data suggest a tooth that has a radiolucent periapical lesion greater than 5 mm will have a decreased long-term success rate for treatment-planned definitive restorations. Investigators have questioned the lack of periapical pathosis or the reduction in radiographic periapical lesion size across time as a criterion for endodontic success, mainly because of limitations in interpretation with the use of 2D periapical radiographs, but also with the advent of the increased sensitivity afforded by 3D CBCT.9 With the growing use of CBCT, the incidence of periapical pathosis in endodontic outcomes studies undoubtedly will increase.9
Gaining CBCT information and establishing clinical guidelines and parameters aids the clinician in diagnosing and treatment planning as well as in case presentation to the patient. The choice presented to the patient is to extract and use an implant or to treat the tooth endodontically. The ability of the CBCT image to measure the size of the lesion digitally and with solid accuracy helps guide the dentist in a decision for the patient. The linear measurement accuracy of CBCT was tested in various units. An evaluation of the accuracy of CBCT found mean differences varying from 0.37 mm to 0.58 mm on CBCT images for linear distances, compared with the actual measurements.10
Biologic Considerations for Implant Placement and Restoration
Various long-term goals for dental implants and associated restorations should be considered within a treatment plan. CBCT images can expedite the process by clearly identifying structures that are necessary to create exceptional esthetic, maintainable restorations and by identifying unforeseen conditions. A fundamental principle that dentists should keep in mind is that implant dentistry is restoratively driven. In addition, the patient either presents with an adequate amount of supporting structures for implant dentistry or does not. How much soft tissue is available? How much bone is available? Is the sinus floor low, and is there enough distance away from the inferior alveolar nerve? How much vertical and buccal-lingual dimensions are available? Does the patient have the appropriate mesiodistal dimensions regarding adjacent natural dentition or previously placed dental implants and restorations to develop soft-tissue architecture and emergence profile from the implant platform? Are there additional pathology, existing defects, or potential occlusal considerations? Does the patient require bone or soft-tissue augmentation? Are short, standard lengths, wide, narrow (mini), or zirconia implants considered in the development of the treatment plan and utilized to the best capacity to avoid sinuses and nerves? Does the patient present with the necessary bone and soft-tissue foundations that are measurable and acceptable for long-term restorations after dental implant placement?
Table 3 shows the combinations and relationships of bone and soft-tissue support in the treatment-plan decision-making for dental implants and final restorations. At the visual oral examination, the clinician observes the soft tissue and determines the soft-tissue profile. Is the visualized tissue thick or thin? The height, buccolingual width, and contour of the ridge can be visually assessed. Careful palpation of the ridge will detect any presence of concavities. If the overlying tissue is fibrous or thicker, accurate assessment may be difficult with visual assessment and palpation.
3D CBCT is the radiograph of choice to identify the amount of bone volume available for an implant to be placed. The width of the available bone cannot be quantified on intraoral radiographs because the view is 2D and must be determined clinically and in conjunction with a CBCT image. Space management is required to provide 1.5 mm of crestal bone interproximally to allow for proper development of healthy papillae,11-13 proper contacts and contours in the restoration, adequate width of soft tissue between implants or adjacent teeth, and prevention of the prosthetic components from impacting each other.14 Preplanning the implant placement is important for optimizing hygiene with effective cleaning of the prosthetics by the patient, along with developing harmonious occlusion and a minimum of 1-mm spacing between the implant and the adjacent natural tooth root.14
Considering the above guidelines, a 4-mm regular platform implant requires a 7-mm mesiodistal space between the adjacent teeth at the coronal region. If an implant is placed too close to the adjacent teeth, compromised contours and unnecessary loss of hard and soft tissue adjacent to the implant will result. Placing the restoration too far from the adjacent tooth also results in unfavorable contours and development of cantilever-type forces on the restoration.
Implant-supported restorations provide considerable advantages over other available treatment options and, therefore, must be considered as a treatment option for restoration of missing teeth. The implant is placed in an optimal position to effectively support the restoration and surrounding soft and hard tissues. The clinician must carefully evaluate all the factors outlined to ensure a long-term predictable outcome, assisted by CBCT radiography.
Treatment Plan After Trauma
A young man presented with a fractured maxillary left-central incisor on a Monday morning after a Saturday evening discussion that did not end well (Figure 1). Visual oral examination and palpation of the structures revealed mobility of 3+, pain on palpation and percussion, a thick soft-tissue profile, and a low lip line. Gingival zeniths were irregular, there was a class II division 2 deep bite, and the periodontium was healthy overall (Figure 2 through Figure 4). Radiographs requested at the time of the initial visit were periapicals, panoramic, and CBCT images (Figure 5 and Figure 6). After all images and information were reviewed and the extent of his injury was discussed, the patient was presented with the following options: removable prosthetics, fixed partial denture, extract and do nothing, or extract and place a dental implant with bone augmentation.
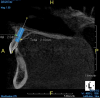
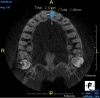
Reviewing the CBCT images with the patient proved beneficial because he was able to clearly see the complete fracture of his tooth in the apical third of the root (Figure 6). Figure 5 represented what is a common radiograph in most dental offices, but it was not clear enough to diagnose a root fracture of this nature. The patient understood that the prognosis was poor and that the long-term restoration he wanted would mimic nature and be maintainable like natural dentition. The visual examination and photographs provided a basis for subsequent dental therapy and a definitive treatment plan for the future. The patient decided to move forward with tooth extraction, grafting, and immediate dental-implant placement with a screw-retained provisional out of occlusion.
Due to the young man's college schedule and consequent time constraints, he was appointed the next day. A surgical guide was not used because there was limited time and there was an appropriate amount of thick soft-tissue profile, measured amount of bone volume based on the CBCT, and virtual placement of the dental implant. Figure 7 and Figure 8 showed the measurements to be more than 2 mm buccal and lingual to the proposed implant placement. The interproximal dimensions mesial and distal to the implant proposal were greater than the 1.5 mm previously mentioned in this article. The CBCT images provided the spatial dimensions and a mental awareness regarding implant placement angulation. The final position was predetermined and acceptable for the considerations necessary in choosing the abutment (zirconia or titanium) and final restoration. Because the implant had appropriate bone length and abundant 360-degree bone volume, minimal augmentation was needed. The natural clinical crown was used to provide an ideal emergence profile to enhance the soft-tissue architecture. Atraumatic tooth extraction was extremely helpful in the development of this treatment plan. Having 1.5 mm to 2 mm of facial bone available after the extraction would facilitate exceptional healing and long-term results. Figure 9, occlusal view, depicted a thick soft-tissue profile and properly placed implant within the arch form.
The CBCT images preoperatively provided the blueprint to execute the therapy and create a pleasant patient experience and meet the expectations of the clinician. After the surgery, a screw-retained provisional crown was fabricated using the patient's natural clinical crown. The provisional was kept out of occlusion in all excursions and full occlusion (Figure 10). At 3 weeks, the patient returned for evaluation of tissue response and occlusion. The soft tissue was responding well, the patient was without pain, and he was able to maintain optimum hygiene. Papillae of the adjacent teeth were intact and the papilla surrounding the implant was developing (Figure 11). The patient would return (4-months postsurgical appointment allowing dental implant osseointegration) to discuss soft-tissue recontouring of the adjacent dentition for cosmetic concerns, final abutment, and final crown-seating appointments.
Conclusions
Imaging is a critically important aspect of diagnostics and treatment planning when placing dental implants. High-quality, accurate images collected at presurgical appointments can optimize success in implant outcomes and patient satisfaction.
Traditional radiographic methods are not ideal for planning implant placement because a clinician is visualizing a 3D object in two dimensions and consequently missing important information. The development of CT allowed clinicians to take radiographic cross-sections, paving the way for 3D reconstructions of maxillofacial features, although this improvement came at the cost of higher radiation exposure.15,16
CBCT is an advancement of the CT technology that uses a cone-shaped x-ray beam and a 2D image receptor to generate high-quality 3D reconstructions with significantly lower radiation exposure.15 Because of these features, the Academy of Oral and Maxillofacial Radiology recommends this technique for presurgical assessments of implant sites.17 This is in accordance with the ALARA principle that radiation exposure should be minimized to produce an image of the required spatial resolution and diagnostic quality.5 Gone are the days when clinicians had to rely on 2D implant-placement planning. Advances in technology have revolutionized the treatment-planning workflow. Clinicians can use 3D reconstructions, such as those based on CBCT scans, to better understand the situation they are correcting and create a prosthetic-driven plan to optimize treatment for each individual patient.
One recent study compared treatment planning using panoramic radiography with the combination of panoramic radiography and CBCT. In that study, performing a CBCT scan during the implant-planning phase increased the agreement in predicting implant length considerably, from 40% after the initial 2D scan to 69.5%.15,16,18,19
Patient benefits of CBCT: An approach that comprises virtual treatment planning using CBCT followed by guided surgery has numerous benefits. In combination with laboratory treatment-planning software and a guided-surgery approach, CBCT allows clinicians to use flapless implant placement, which is less invasive and associated with high patient satisfaction20-22 and reduced patient discomfort,23-25 and it also has improved soft-tissue outcomes.26
In summary, by incorporating CBCT into the workflow for planning guided surgeries, one can reduce the number of chairside decisions that must be made during surgery, improve surgical outcomes, and increase patient satisfaction.
About the Author
Thomas M. Bilski, DDS
Private Practice
Independence, Ohio
References
1. Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006;35(4):219-226; erratum in Dentomaxillofac Radiol. 2006;35(5):392.
2. Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006;72(1):75-80.
3. Bamgbose BO, Adeyemo WL, Ladeinde AL, Ogunlewe MO. Conebeam computed tomography (CBCT): the new vista in oral and maxillofacial imaging. Nig Q J Hosp Med. 2008;18(1):32-35.
4. Stuehmer C, Essig H, Bormann KH, et al. Cone beam CT imaging of airgun injuries to the craniomaxillofacial region. Int J Oral Maxillofac Surg. 2008;37(10):903-906.
5. Radiation and your health. ALARA - As Low As Reasonably Achievable. CDC. https://www.cdc.gov/nceh/radiation/alara.html. Updated December 7, 2015. Accessed April 11, 2018.
6. Sadiq Z, Bisase B, Coombes DM. Use of cone beam computed tomography in the management of glass injuries to the face. Br J Oral Maxillofac Surg. 20010;48(4):308-309.
7. Misch CE, ed. Contemporary Implant Dentistry. St. Louis, MO: Mosby; 1993.
8. Kendrick S, Wong D. When to restore or extract-a clinical guide. Inside Dentistry. 2011;7(1):42-50.
9. Bernstein SD, Horowitz AJ, Man M, et al. Outcomes of endodontic therapy in general practice: a study by the Practitioners Engaged in Applied Research and Learning Network. J Am Dent Assoc. 2012;143(5):478-487.
10. Moshfeghi M, Tavakoli MA, Hosseini ET, et al. Analysis of linear measurement accuracy obtained by cone beam computed tomography (CBCT-NewTom VG). Dent Res J (Isfahan). 2012;9(suppl 1):S57-S62.
11. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(suppl):43-61.
12. Belser U, Buser D, Higginbottom F. Consensus statements and recommended clinical procedures regarding esthetics in implant dentistry. Int J Oral Maxillofac Implants. 2004;19(suppl):73-74.
13. Kois JC. Predictable single-tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2004;25(11):895-900.
14. Floyd P, Palmer R, Barrett V. Dental implants. 4. Treatment planning for implant restorations. Br Dent J. 1999;187(6):297-305.
15. Sukovic P. Cone beam computed tomography in craniofacial imaging. Orthod Craniofac Res. 2003;6(suppl 1):31-36; discussion 179-182.
16. Tsiklakis K, Donta C, Gavala S, et al. Dose reduction in maxillofacial imaging using low dose cone beam CT. Eur J Radiol. 2005;56(3):413-417.
17. Tyndall DA, Price JB, Tetradis S, et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(6):817-826.
18. Benavides E, Rios HF, Ganz SD, et al. Use of cone beam computed tomography in implant dentistry: the International Congress of Oral Implantologists consensus report. Implant Dent. 2012;21(2):78-86.
19. Chan HL, Misch K, Wang HL. Dental imaging in implant treatment planning. Implant Dent. 2010;19(4):288-298.
20. Farman AG. ALARA still applies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(4):395-397.
21. Mello LA, Garcia RR, Leles JL, et al. Impact of cone-beam computed tomography on implant planning and on prediction of implant size. Braz Oral Res. 2014;28:46-53.
22. van Steenberghe D, Glauser R, Blombäck U, et al. A computed tomographic scan-derived customized surgical template and fixed prosthesis for flapless surgery and immediate loading of implants in fully edentulous maxillae: a prospective multicenter study. Clin Implant Dent Relat Res. 2005;7(suppl 1):S111-S120.
23. Abad-Gallegos M, Gómez-Santos L, Sánchez-Garcés MA, et al. Complications of guided surgery and immediate loading in oral implantology: a report of 12 cases. Med Oral Patol Oral Cir Bucal. 2011;16(2):e220-e224.
24. Yamada J, Kori H, Tsukiyama Y, et al. Immediate loading of complete-arch fixed prostheses for edentulous maxillae after flapless guided implant placement: a 1-year prospective clinical study. Int J Oral Maxillofac Implants. 2015;30(1):184-193.
25. Pozzi A, Tallarico M, Marchetti M, et al. Computer-guided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomised controlled trial. Eur J Oral Implantol. 2014;7(3):229-242.
26. Nkenke E, Eitner S, Radespiel-Tröger M, et al. Patient-centred outcomes comparing transmucosal implant placement with an open approach in the maxilla: a prospective, non-randomized pilot study. Clin Oral Implants Res. 2007;18(2):197-203.