You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Teeth with symptoms of pain or temperature sensitivity (ie, prolonged and exacerbated by heat) or that have periapical pathology as evidenced radiographically may require endodontic intervention to preserve their structure. When clinical findings can be linked to pulpal pathology, a tooth must be evaluated from a periodontal and restorative standpoint before endodontic treatment is initiated.
The practitioner must determine whether the tooth is periodontally stable or can, with elimination of the infection associated with the pulp and apical tissue, become periodontally stable. Even more importantly, it must be determined whether the tooth can be restored predictably after endodontic treatment. Identifying the canals, instrumenting them, and obturating the canal system is not important if the tooth cannot be restored and preserved predictably. Therefore, diagnosis of endodontically involved teeth must be restoratively driven. This article will look at the various steps of endodontic treatment and how, from a restorative standpoint, treatment can be improved for better long-term predictability.
Endodontic Access: Preservation of Tooth Structure
Preservation of tooth structure is critical for long-term survival of the tooth, especially in the cervical zone.1 When teeth are loaded under function, stress concentrates in the cervical area (Figure 1).2 Frequently, endodontically treated teeth require restoration with a crown or onlay due to the missing tooth structure related to decay or previous restorative materials (amalgam and composite). Decay must be removed, as well as previously placed restorative materials. However, the practitioner can attempt to preserve as much of the remaining tooth structure as possible; fundamental to this process is access for initiation of endodontics.
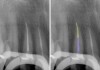
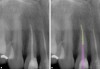
Indiscriminate removal of tooth structure by hunting for the canal orifices when anatomy is either not understood or ignored weakens the tooth, specifically in the cervical area, where exploration occurs when trying to find the orifices. Understanding tooth anatomy and the location of the canal orifices in relation to that anatomy aids in preserving tooth structure, especially in the cervical region (Figure 2). The process can become a challenge when endodontically treating a tooth with a previously placed crown because the practitioner may lose orientation of the anatomy due to the restoration having corrected tooth rotation, tipping, or other positional changes. Ideally, the objective is to remove minimal tooth structure with only what is necessary to identify the canal orifices and provide straight-line access into each canal in the tooth. After isolation with a rubber dam, all decay is removed from the tooth to be treated, as well as old restorative materials present that may limit canal access. A pre-endodontic buildup may be performed to reinforce the remaining tooth structure and allow clamp placement with access into the canals (Figure 3).3
Instrumentation
Rotary nickel-titanium (NiTi) files have greatly improved the quality and precision of endodontic treatment. However, hand files are still a good initial starting point to achieve a glide path to the canals' working length (WL). After a glide path has been achieved, fracture of the NiTi file is a rare occurrence as long as the rotary file is not forced apically in the canal, which can result in binding within the canal, especially in calcified or moderately curved canals.
After identification of the canal orifice, a carbon steel hand file with a 1% taper and square in cross-section should be introduced into the canal to the estimated working length (eg, Dia-Probe file, DiaDent®, diadent.com; Pathfinder™ CS, Sybron Endo, kerrdental.com; Pathglider™, Komet USA, kometUSA.com) (Figure 4 and Figure 5). Use of an ethylene diamine tetra acetic acid (EDTA)-based canal lubricant (eg, DiaPrep™ Pro, DiaDent; RC-Prep®, Premier Dental, premusa.com; Glyde™, Dentsply, dentsplysirona.com) facilitates apical advancement of the file to WL. EDTA, a calcium chelating agent, softens calcifications that may hamper file advancement.4 If introduction of the hand file into the canal orifice is hampered due to calcification, a rotary orifice opener may be implemented (eg, DiaPrep™ Pro, DiaDent; RC-Prep®, Premier Dental, premusa.com; Glyde™, Dentsply, dentsplysirona.com). Orifice openers equivalent to an International Organization for Standardization (ISO) #16 file with a 0.04 taper are designed to be used in the coronal half of the canal to aid in bypassing calcifications that prevent file advancement to the WL. After WL has been reached, the file should be moved in a coronal apical direction until a loose fit of the file occurs. For canals that are calcified, use of NiTi K-file hand files is recommended (eg, from DiaDent, Komet, or Dentsply), advancing from a #8 to #20 before introduction of a rotary file. The benefit of NiTi hand files compared with stainless steel files is that NiTi has greater stress resistance, leading to decreased potential for file separation in calcified and curved canals. Additionally, the higher flexibility of the NiTi hand files allows better negotiation, with less potential of canal zipping or transportation.
With conservative preparation in mind, one needs to consider taper of the rotary file. Excessive enlargement of the canal in the coronal third may internally weaken the tooth at the cervical region. The initial canal diameter as measured by a hand file in the apical half of the root should be used to gauge the final instrumentation size. In the author's opinion, the majority of canals can be finished with an ISO #25/0.07 file (eg, D4, Dia-X; Hyflex; TF™ Adaptive, Sybron Endo); however, canals that are typically large (palatal of maxillary molars, distal of mandibular molars, maxillary central incisors, and all canines) will require a #35/0.08 file (eg, D5, Dia-X; Hyflex; TF Adaptive) for proper instrumentation and cleaning of the canal in preparation for obturation (Figure 6). Mandibular incisors, especially in older patients, may only permit instrumentation up to a #20/0.06 file (eg, D3, Dia-X; Hyflex; TF Adaptive). Periodically, canals may be encountered that are larger than a final file size of #35; these can be finished with that file and a reciprocating motion as the file is worked against the canal walls circumferentially.
Advances in how NiTi is manufactured have greatly improved the properties of the resulting files. NiTi alloys that have been thermomechanically treated have been reported to offer greater flexibility, with improved cyclic fatigue resistance compared with conventional NiTi.5 Controlled memory technologies have increased the fatigue resistance of rotary NiTi files.6 Additionally, coatings applied by the manufacturer have improved resistance to corrosion, which may occur through sodium hypochlorite (NaOCl) contact, hence improving fracture resistance during use, specifically at the terminal end of the file. The coatings have also been reported to improve cutting efficiency, with a high resistance to corrosion and a better performance in fatigue life after corrosion.7 Files with a non-cutting tip are less likely to transport the canal, cause zipping, or perforate the tooth during use. Some files incorporate these advances with a non-cutting tip and convex triangular cross-section, which reduces rotational friction and contact with the canal wall, decreasing potential to bind within the canal, without sacrifice to instrumentation efficiency (Figure 7).
Irrigation
The main objective of endodontic therapy is the removal of necrotic tissue (pulp) and bacteria within the canal system. Irrigation is crucial for successful endodontic treatment and is a counterpart to proper instrumentation. Endodontic files, be they hand files or rotary, are unable to access the entire canal system and are confined to the main canals present. Lateral canals, anastomosis, fins, and other canal anatomy off the main canals cannot be instrumented with files; to remove pulpal tissue from these areas, irrigation is required (Figure 8). Irrigants reduce friction between the instrument and dentin, improving cutting efficiency of the files while dissolving tissue, and have an antimicrobial/antibiofilm effect. Irrigation is also the only way to reach areas of the root canal wall that are not touched by mechanical instrumentation.
During endodontic treatment, two different tissues are encountered in the instrumentation phase of care, pulpal (soft tissue) and dentin (hard tissue). Each requires a different approach to managing and allowing the canal system to be fully cleaned. NaOCl has a long history in endodontic use for dissolution and removal of pulpal tissue. Currently, no other irrigant has the same tissue dissolution ability on pulpal tissue within the canal system.8There has been ongoing debate regarding temperature and concentration of NaOCl and its effectiveness. Temperature variation of NaOCl has been shown not to be relevant in killing or dissolving bacterial biofilms; concentration appears to be a more relevant factor.9 Higher concentrations are more effective in tissue dissolution than lower concentrations, so diluting the NaOCl negatively affects its intended use.10,11 Contact time in the canal system is also important; scientific literature supports use of higher concentrations (5.25%) with longer contact times when instrumentation is carried out with NaOCl in the canals and pulp chamber. Enterococcus faecalis is a common type of bacteria found intraorally; it has been routinely identified in the canal system and is difficult to remove during instrumentation and irrigation when NaOCl concentration and contact time are inadequate.12 No evidence has been supplied that other irrigants are effective against E. faecalis, and residual levels of this bacteria can be associated with endodontic failure.
Yet, with the complex anatomy of the canal system and limited ability to instrument the entire system, NaOCl on its own cannot reach completely into the anatomy within the tooth. The apical root canal imposes special challenges to irrigation as a balance between safety and effectiveness. Use of a rotary file or ultrasonics in the canal filled with NaOCl aids in delivery of the irrigant to that region and removal of pulpal tissue and bacteria that may lead to a recurrent infection after obturation. EDTA will soften and dissolve dentin within the canal system, allowing better penetration and tissue removal by NaOCl. A 17% EDTA solution (eg, Endo-Clear™, DiaDent; Endo-Cleanse, Roydent™, roydent.com; EDTA solution, Vista™, vista-dental.com) that has been alternated with NaOCl allows the anatomy to be opened and deeper tissue removal to occur, following the axiom that only one thing can occupy a space at a time; if residual tissue is present, sealer cannot fill that anatomy, so remaining bacteria can lead to failure. Because the EDTA is not left in the canal system for long periods (it is used for a single file before irrigant removal and placement of NaOCl for the next file), no erosion on the dentinal tubules has been reported.13 Additionally, EDTA assists in smear layer removal in the canal system.
With resin-based sealers (eg, AH-26®, Dentsply; Adseal™, Meta Biomed, metabiomedamericas.com; EndoRez®, Ultradent, ultradent.com), dentin bond strength can be affected by NaOCl remaining in the canal system.14,15 However, EDTA as the final irrigant has been shown not to affect bond strength and appears to improve flow and adaption of the sealer to the dentin surfaces in the canal system.16 Better adaption of the sealer will decrease leakage potential coronally and apically and will improve treatment success. An increase in resin sealer bond strength when EDTA was used as the final irrigant before obturation has also been reported.17 Use of chlorhexidene (CHX) as a final irrigant has no reported negative effects on bond strength of resin sealer, and some studies have actually shown bond strength improves as a result of its use in the canal system.18
Temporization: Single- or Multiple-Visit Endodontic Treatment
The treatment goal in endodontics is to complete the instrumentation and obturation in a single visit. However, there are clinical situations in which that may not be possible or prudent. Patients who present with pain and an associated periapical lesion or a canal that continues to bleed or exudate flow are better treated in multiple visits. The important factor is to complete instrumentation and irrigation at the first appointment to remove residual bacteria that are contributing to the infection present and allow the body to heal what is outside the root.
Calcium hydroxide (CaOH2) has been used for many years as a canal medicament between appointments due to its antibacterial properties and apical wound healing enhancement. Infections raise the pH apically and within the canal system, favoring the bacteria involved in the infection.19 CaOH2 has a high pH (12.4), neutralizing the bacterial-induced acid environment.20 It is available as a white powder that is mixed with saline, water, or another appropriate liquid to form a paste and is then introduced into the canal system. When insufficient liquid is mixed with the powder, the resulting paste may be too thick to place in the tooth's apical area. A spiral filler (eg, Dia-Spiral Filler, DiaDent; Dyna® paste filler, Thomas, thomas-dentaltools.com; SensiPast®, Premier Dental) can be used to aid in placement of the CaOH2 paste in the apical aspects of the canal system. CaOH2 is radiopaque, so verification that it has been placed to the WL can occur. These types of pastes tend to dry within the canal and may not be easily removed, requiring files, water, and time. Additionally, because they are white in color, it may be difficult to verify other than radiographically that it has been completely removed from the canal system.
Premixed CaOH2 pastes overcome the negatives associated with the powder formulation that requires mixing. These CaOH2 pastes (eg, Diapex®, DiaDent; Vitapex®, Neo Dental, neodental-intl.com) are provided in a prefilled syringe and incorporate CaOH2 (30%), iodoform (40%), and silicone oil (22%) into a non-setting paste. The iodoform improves the antibacterial properties and imparts a bright yellow color to the resulting paste.21 The combination of CaOH2, iodoform, and silicone oil stimulates healing of periapical lesions and induces bone regeneration to promote better healing.22,23 The silicone oil creates a creamy, smooth paste that does not harden over time. Removal from the canal system is performed with water and a rotary file to WL. Verification of removal of the paste is confirmed with a paper point introduced into the canal. Any yellow on the paper point indicates paste still remains in the canal and further irrigation and use of the rotary file is required. An alternative paste (Diapaste™, DiaDent) is available that is iodoform-free with barium sulfate (for patients sensitive to iodoform) and is also water-soluble.
Sealing the access opening, whether between endodontic treatment visits or at completion of endodontic treatment (before restorative treatment can be initiated), is critical to prevent coronal leakage, which may allow bacterial progression from saliva to the periapical area, leading to treatment failure. Ideally, the temporary sealing material should be durable (able to resist the patient functioning on it), seal marginally to prevent leakage, and be relatively easy to remove when treatment is continued. Not all temporary materials fulfill these desired properties. Glass-ionomers, although adhesive and durable, have been reported to leak when used to seal endodontic access and should be avoided in this application.24 Premixed zinc oxide/calcium sulfate temporary putty materials (eg, e-Temp™, DiaDent in Canada; Cavit™, 3M, 3m.com; Tempit®, Centrix, centrixdental.com) are moisture-activated, with slight expansion providing a durable provisional seal of the access opening.25 The provisional filling must be of adequate thickness to provide a seal that mastication will not disrupt.26
Obturation
Removal of any moisture in the canal is the first step in the obturation process. Use of paper points is the standard method; paper points that match the final file ensure that canal drying is more efficient, with fewer points required to complete the task (Figure 9). When a resin sealer is being used, residual moisture in the canal may affect sealer adaption to the canal walls and its adhesion, which can lead to leakage concerns over time.27
Endodontic sealer is considered to be more important than the core obturating material itself. Sealer with the least film thickness is favorable to minimize microleakage. When obturating the canal system, minimal sealer should be used, with the majority of the canal being filled with gutta-percha. Use of a single gutta-percha cone that matches the geometry of the final file used in the canal aids in achieving that goal.28 Additionally, with a single cone matching the last file used, the file by hydraulic force is able to drive the sealer into accessory anatomy that the irrigation protocol removed (Figure 10).
When extensive canal anatomy is present, as observed radiographically, warm vertical compaction may be a better obturation technique than a single-cone approach to achieve a 3-dimensional fill (Figure 11).29 In teeth with extensive canal anatomy, warm vertical compaction appeared to provide better sealing of the canal system than the single-cone obturation when dye penetration studies were performed on extracted teeth.30 Therefore, selection of obturation technique should be based on anatomy of the canal system as well as size of the apical half of the canal. Canals that offer some "tug-back" on a cone that matches the final file size can be predictably obturated with a single cone, whereas when there is no tug-back and shortening the cone at the apical end does not achieve that, a warm vertical compaction should be selected.
Sealer is placed into the canal with a sized paper point to ensure that excessive sealer is not forced out periapically. The tip of a gutta-percha gun (eg, Duo-Gun, DiaDent; GPO, Cicada Dental, cicadadental.com; Elements™, Sybron Endo) (Figure 12) is inserted into the canal, and heated gutta-percha is extruded as the tip is withdrawn, leaving a small portion of warm gutta-percha in the canal at the apical. A condenser (eg, Dia-Kondensor, DiaDent; Buchanan Hand Plugger, Sybron Endo; Finger Plugger, Brasseler, brasselerusa.com) that is sized to the final file size is immediately inserted into the canal to WL to compact the warm obturation material. A radiograph is taken to verify apical seal, and the gutta-percha gun is used to backfill the canal to the orifice, with additional compaction with a hand instrument. As an alternative technique, a single cone can be placed with sealer to WL and the cone cut off and condensed in the canal with a heated pen-like instrument (eg, Duo-Pen, DiaDent; Elements, Sybron Endo; Thermique™, Parkell, parkell.com) (Figure 13). The remaining canal system is backfilled with warm gutta-percha and further condensed, completely filling the canal anatomy (Figure 14). The pen instrument also aids in post preparation by assisting in removal of the obturation material before use of a post drill. This decreases the potential to divert from the canal trajectory as the post drill then follows the hole in the obturation material just created.
Restoration: To Post or Not to Post
Controversy still exists with regard to use of posts in teeth. However, depending on what remaining tooth structure is present, a post may be indicated to aid in retention of the core.31 Teeth that have both marginal ridges intact may only require an adhesive direct resin as the final restoration.32 When one or both marginal ridges are missing, a laboratory-fabricated restoration (crown or onlay) may best preserve the tooth. When significant portions of the native tooth structure will be missing after crown preparation, the tooth would benefit from a post to aid in retention of the core (Figure 15). Endodontically treated teeth restored with composite or composite combined with fiber posts have resisted fatigue tests and currently represent the best treatment option. In comparison with rigid metal posts, when composite and fiber posts fail, catastrophic failure of the tooth is less likely.33 The main factor in use of a post is to preserve tooth by not over-preparing the post preparation. The post preparation should be similar in size to the coronal canal preparation that was performed when the tooth was endodontically instrumented (Figure 16). This will conserve important tooth structure in the cervical region.
Ferrule is also important, even in the age of adhesive dentistry. Teeth under function, especially the maxillary anterior, will have micro-movement in the buccal-lingual direction. In the absence of a restorative ferrule, the marginal seal will potentially open over time, leading to recurrent decay, dislodgement of the crown, or fracture of the remaining underlying tooth. Non-ferrule teeth show increased root dentin strain, whereas teeth with ferrule reveal higher fracture resistance, lower stress concentration on root dentin, and fewer catastrophic fractures.34 This is supported in scientific literature: ferrule-containing endocrown preparations have demonstrated significantly greater failure loads than those with decreased ferrule height. Ferrule of 2 mm appears to offer the best resistance to loading failures under function (Figure 17).35,36
Conclusion
Before initiation of endodontic treatment, a tooth must be evaluated from a restorative standpoint. Preservation of tooth structure, especially in the cervical region, may determine the longevity of that tooth under function. Will there be adequate tooth structure remaining after decay removal and treatment to predictably restore that tooth? Conservative access to initiate endodontic treatment, removing only necessary dentin to identify the canal orifices and allow straight-line access, is the start of restorative-driven endodontics. Rotary NiTi has improved the efficiency and quality of treatment; use of a final file size that does not over-prepare the canal will not weaken the tooth. Irrigation is a crucial counterpart to quality instrumentation because it aids in debris removal and clearing of parts of the canal system that the file is unable to reach. The cleaner the canal system, the better the obturation and resulting decreased leakage potential, which will improve treatment success. Restoration of these teeth must be approached from an engineering standpoint, and the best way to achieve that is preservation of as much native tooth structure as possible, especially in the cervical region, where loading stress is concentrated.
About the Author
Gregori M. Kurtzman, DDS, MAGD
Private Practice
Silver Spring, Maryland
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Jiang W, Bo H, Yongchun G, LongXing N. Stress distribution in molars restored with inlays or onlays with or without endodontic treatment: a three-dimensional finite element analysis. J Prosthet Dent. 2010;103(1):6-12.
2. McCoy G. Occlusion fails. Dent Today. 2015;34(12):8,10.
3. Kurtzman G. Improving endodontic success through coronal leakage prevention. Inside Dentistry. 2005;1(2). https://www.aegisdentalnetwork.com/id/2005/12/endodontics-improving-endodontic-success-through-coronal-leakage-prevention. Accessed August 23, 2018.
4. Stewart GG. Gaining access to calcified canals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79(6):764-768.
5. Zupanc J, Vahdat-Pajouh N, Schäfer E. New thermomechanically treated NiTi alloys - a review. Int Endod J. 2018. doi: 10.1111/iej.12924.
6. Braga LC, Faria Silva AC, Buono VT, de Azevedo Bahia MG. Impact of heat treatments on the fatigue resistance of different rotary nickel-titanium instruments. J Endod. 2014;40(9):1494-1497.
7. Aun DP, Peixoto IFDC, Houmard M, Buono VTL. Enhancement of NiTi superelastic endodontic instruments by TiO2 coating. Mater Sci Eng C Mater Biol Appl. 2016;68:675-680.
8. Amato M, Pantaleo G, Abtellatif D, et al. An in vitro evaluation of the degree of pulp tissue dissolution through different root canal irrigation protocols. J Conserv Dent. 2018;21(2):175-179.
9. Del Carpio-Perochena A, Monteiro Bramante C, Hungaro Duarte M, et al. Effect of temperature, concentration and contact time of sodium hypochlorite on the treatment and revitalization of oral biofilms. J Dent Res Dent Clin Dent Prospects.2015;9(4):209-215.
10. Haapasalo M, Shen Y, Wang Z, Gao Y. Irrigation in endodontics. Br Dent J. 2014;216(6):299-303.
11. Siqueira JF Jr, Rôças IN, Favieri A, Lima KC. Chemomechanical reduction of the bacterial population in the root canal after instrumentation and irrigation with 1%, 2.5%, and 5.25% sodium hypochlorite. J Endod.2000;26(6):331-334.
12. Retamozo B, Shabahang S, Johnson N, et al. Minimum contact time and concentration of sodium hypochlorite required to eliminate Enterococcus faecalis. J Endod. 2010;36(3):520-523.
13. Li C, Du R, Zhu YQ. Comparison of the effects of 5 irrigant combinations on cleaning of anterior straight root canal walls. [article in Chinese] Shanghai Kou Qiang Yi Xue. 2005;14(3):293-297.
14. Cecchin D, Farina AP, Bedran-Russo AK. The effects of endodontic substances and naturally reducing agents on the bond strength of epoxy resin-based sealer to root dentin. J Conserv Dent. 2017;20(5):302-306.
15. Prado M, Simão RA, Gomes BP. Effect of different irrigation protocols on resin sealer bond strength to dentin. J Endod. 2013;39(5):689-692.
16. Mohan RP, Pai AR. The comparison between two irrigation regimens on the dentine wettability for an epoxy resin based sealer by measuring its contact angle formed to the irrigated dentine. J Conserv Dent. 2015;18(4):275-278.
17. Vilanova WV, Carvalho-Junior JR, Alfredo E, et al. Effect of intracanal irrigants on the bond strength of epoxy resin-based and methacrylate resin-based sealers to root canal walls. Int Endod J. 2012;45(1):42-48.
18. Dinesh K, Murthy BV, Narayana IH, et al. The effect of 2% chlorhexidine on the bond strength of two different obturating materials. J Contemp Dent Pract.2014;15(1):82-85.
19. Kim D, Kim E. Antimicrobial effect of calcium hydroxide as an intracanal medicament in root canal treatment: a literature review - Part I. In vitro studies. Restor Dent Endod. 2014;39(4):241-252.
20. Mohammadi Z, Jafarzadeh H, Shalavi S, et al. Additive and reducing effects between calcium hydroxide and current irrigation solutions. J Contemp Dent Pract.2017;18(3):246-249.
21. Du TT, Qiu LH, Jia G, et al. Antimicrobial effect of various calcium hydroxide on Porphyromonas endodontalis in vitro. [article in Chinese] Shanghai Kou Qiang Yi Xue. 2012;21(2):149-153.
22. Al Khasawnah Q, Hassan F, Malhan D, et al. Nonsurgical clinical management of periapical lesions using calcium hydroxide-iodoform-silicon-oil paste. Biomed Res Int. 2018;2018:8198795. doi: 10.1155/2018/8198795.
23. Xia X, Man Z, Jin H, et al. Vitapex can promote the expression of BMP-2 during the bone regeneration of periapical lesions in rats. J Indian Soc Pedod Prev Dent. 2013;31(4):249-253.
24. Srivastava PK, Nagpal A, Setya G, et al. Assessment of coronal leakage of temporary restorations in root canal-treated teeth: an in vitro study. J Contemp Dent Pract. 2017;18(2):126-130.
25. Balto H, Al-Nazhan S, Al-Mansour K, et al. Microbial leakage of Cavit, IRM, and Temp Bond in post-prepared root canals using two methods of gutta-percha removal: an in vitro study. J Contemp Dent Pract. 2005;6(3):53-61.
26. Aledrissy HI, Abubakr NH, Ahmed Yahia N, et al. Coronal microleakage for readymade and hand mixed temporary filling materials. Iran Endod J. 2011;6(4):155-159.
27. Nagas E, Uyanik MO, Eymirli A, et al. Dentin moisture conditions affect the adhesion of root canal sealers. J Endod. 2012;38(2):240-244.
28. Setya G, Nagpal A, Kumar S, Ingle NA. Comparison of root canal sealer distribution in obturated root canal: an in-vitro study. J Int Soc Prev Community Dent. 2014;4(3):193-197.
29. Barbosa FO, Gusman H, Pimenta de Araújo MC. A comparative study on the frequency, location, and direction of accessory canals filled with the hydraulic vertical condensation and continuous wave of condensation techniques. J Endod. 2009;35(3):397-400.
30. Robberecht L, Colard T, Claisse-Crinquette A. Qualitative evaluation of two endodontic obturation techniques: tapered single-cone method versus warm vertical condensation and injection system: an in vitro study. J Oral Sci. 2012;54(1):99-104.
31. Vadavadagi SV, Dhananjaya KM, Yadahalli RP, et al. Comparison of different post systems for fracture resistance: an in vitro study. J Contemp Dent Pract. 2017;18(3):205-208.
32. von Stein-Lausnitz M, Bruhnke M, Rosentritt M, et al. Direct restoration of endodontically treated maxillary central incisors: post or no post at all? Clin Oral Investig. 2018. doi: 10.1007/s00784-018-2446-6.
33. Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies). Quintessence Int. 2008;39(2):117-129.
34. Valdivia ADCM, Rodrigues MP, Bicalho AA, et al. Biomechanical effect of ferrule on incisors restored with a fiberglass post and lithium-disilicate ceramic crown after thermal cycling and fatigue loading. J Adhes Dent. 2018;20(2):133-142.
35. Einhorn M, DuVall N, Wajdowicz M, et al. Preparation ferrule design effect on endocrown failure resistance. J Prosthodont. 2017. doi: 10.1111/jopr.12671.
36. Ichim I, Kuzmanovic DV, Love RM. A finite element analysis of ferrule design on restoration resistance and distribution of stress within a root. Int Endod J. 2006;39(6):443-452.